From IEEE Spectrum Dec2020 — The no-contact temperature screening systems can be off as much as four degrees –
Editors Note: this is Erik Beall writing this article and we believe his company offers fever inspection products. We cannot vouch for the accuracy of his testing as it has not been confirmed. Much of the text is a good read thru and explanation of the at best confusing policies of the FDA.
THE INSTITUTE As part of the effort to curb the spread of the coronavirus, countries have implemented body-temperature screenings at airports, train stations, and other public spaces to detect fever. Many of the systems include the use of infrared (IR), or thermographic, cameras such as those featured in The Institute article “Thermal Cameras Are Being Outfitted to Detect Fever and Conduct Contact Tracing for COVID-19.”
The market has been flooded with infrared fever-screening products, but almost none has undergone independent testing. Demand has been so great, many companies rushed into the field without understanding the accuracy requirements, and they’ve used technology that cannot possibly measure body temperature well enough. In many cases, their products are unable to tell the difference between core temperatures of 35 and 40 °C, or distinguish between hypothermia and a severe fever.
CURRENT SCREENING METHODS
There are three types of fever screenings commonly used in North America. Each comes with its own limitations.
Clinicians typically use oral thermometers during medical visits. Unfortunately, high-quality clinical-grade thermometers are not widely available. Furthermore, it’s not efficient or safe to use them outside clinical environments, because the operator needs to be in close proximity to possibly infected people. Also, if people drink something hot or cold before getting their temperature taken or cannot breathe through their nose and must open their mouth, that will affect the results.
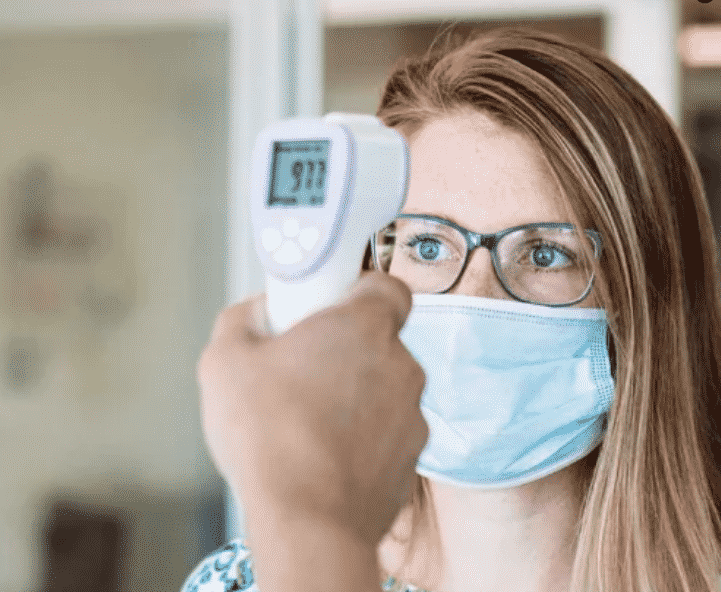
Noncontact infrared thermometers (NCITs), commonly known as forehead screeners, are being used at fitness centers, schools, and businesses. Many of you probably have had your temperature taken by one recently.
Some NCITs, including those with U.S. Food and Drug Administration approval, struggle to tell the difference between people with hypothermia (35 °C) and those with a severe fever (40 °C), even when operated properly in a controlled environment.
Even though NCIT sensors are accurate, they don’t account for how air temperature affects their measurements. NCITs also must be operated at a consistent distance to their target, and unfortunately foreheads vary too much. If NCITs were to report temperatures in real-world conditions, often they would be absurd. Some devices do report absurd readings, while others seem to report close-to-normal temperatures most of the time. The latter devices might do a lot of averaging of temperatures. For whatever reason, some manufacturers apparently have decided that rather than figure out how to get accurate readings, they could fudge the numbers and no one would be likely to notice.
Some operators do report the ridiculous readings, while others simply ignore impossibly low readings. That makes many NCITs useless for clinical purposes. Unfortunately, though, because NCITs are the easiest thermometers to obtain, many businesses use them to meet local government requirements.
The thermal imaging field is where we are seeing lots of new products hit the market. The products can work from a safe distance automatically. Near room temperature, everything is glowing in the far infrared electromagnetic spectrum by an amount proportional to its emissivity. Thermal sensing can detect and convert the measured light into a temperature.
An NCIT uses a single pixel sensor, but it must average all temperatures it sees in its field of view—which is why it must be operated so close to the skin. Thermal-imaging systems, on the other hand, use an array of identical pixel sensors to produce images of the luminous intensity, or amount of thermal light falling on each pixel per second per solid angle. To take someone’s temperature, an infrared device must first acquire an accurate surface temperature measurement of a patch of skin. Core body temperature can then be extrapolated, using a previously calibrated relationship between the skin temperature, air temperature, and core body temperature.
The system works because there is a consistently thin level of insulation between core blood and air at the inner canthus—often referred to as the tear duct—the region where the eye meets the bridge of the nose.
In our studies and in data reported by other researchers, we know the surface temperature tracks the core temperature but is reduced by a predictable fraction of the difference between core and ambient air temperature. In fact, a 4 °C change in the room air temperature will change the core temperature reading by a full 1 °C.
Despite manufacturer claims, no thermal imager has been through the FDA’s device-approval process specifically for fever screening. Because of the urgent need for devices that could help fight the pandemic, the FDA released guidance in April declaring the agency did not intend to object to the sale and use of thermal-imaging devices.
However, the agency stated that such devices should (not must) follow an established standard (IEC 80601-2-59:2017) and technical report (ISO/TR 13154:2017) for thermographic fever detection. The standards were designed to minimize mistakes in performing fever detection using off-the-shelf thermographic cameras and IR calibration equipment; no device existed that was explicitly designed for that purpose.
Following the standards, however, is no guarantee the system will be able to detect feverish temperatures reliably. For example, the ISO standard allows the device to take measurements in the same manner even if air temperature changes as much as 4 °C. As discussed before, such a change will throw off the measurement enough to miss mild fevers or have at least a 50 percent false-positive rate.
Nevertheless, thermal imaging is the most promising technology, because it can operate automatically from a safe distance and, importantly, has no additional per-scan costs.
Read full article From IEEE Spectrum Dec2020 –